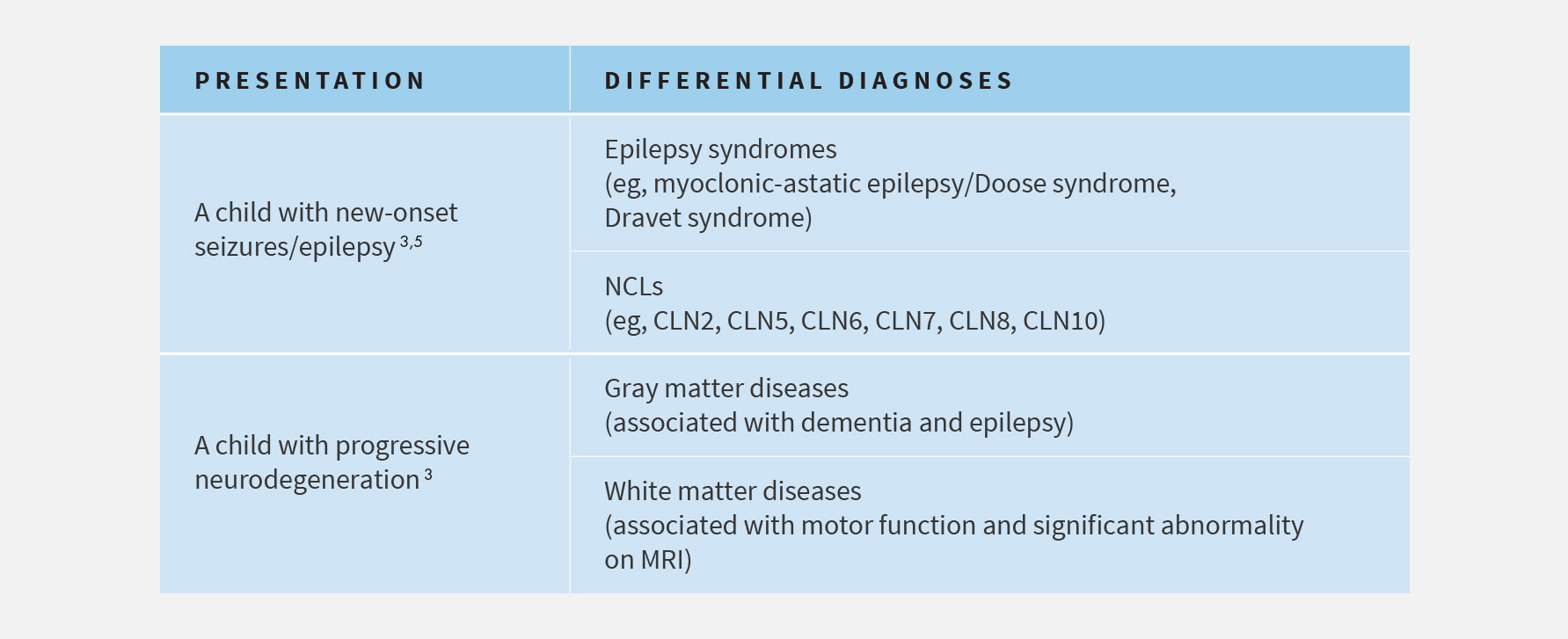
Need for Early Diagnosis
References: 1. Fietz M, Giugliani R, AlSayed M, et al. Expert recommendations for the laboratory diagnosis of neuronal ceroid lipofuscinosis type 2 (CLN2 disease): diagnostic algorithm and best practice guidelines for a timely diagnosis. Poster session presented at: The 12th Annual WORLD Symposium; February – March 2016; San Diego, CA. 2. Williams RE, Adams HR, Blohm M, et al. Expert opinion on the management of CLN2 disease. Poster session presented at: The 12th Annual WORLD Symposium; February – March 2016; San Diego, CA. 3. Chang M, Cooper JD, Davidson BL, et al. CLN2. In: Mole S, Williams R, and Goebel H, eds. The neuronal ceroid lipofuscinoses (Batten Disease). 2nd ed. Oxford, United Kingdom: Oxford University Press; 2011:80-109. 4. Pérez-Poyato MS, Marfa MP, Abizanda IF, et al. Late infantile neuronal ceroid lipofuscinosis: mutations in the CLN2 gene and clinical course in Spanish patients. J Child Neurol. 2013;28:470-478. 5. Mole SE, Williams RE, and Goebel HH. Correlations between genotype, ultrastructural morphology and clinical phenotype in the neuronal ceroid lipofuscinoses. Neurogenetics. 2005;6:107-126.
 Español
Español UK (English)
UK (English) Deutsch
Deutsch Italiano
Italiano Русский
Русский Français
Français