Clinical evaluations
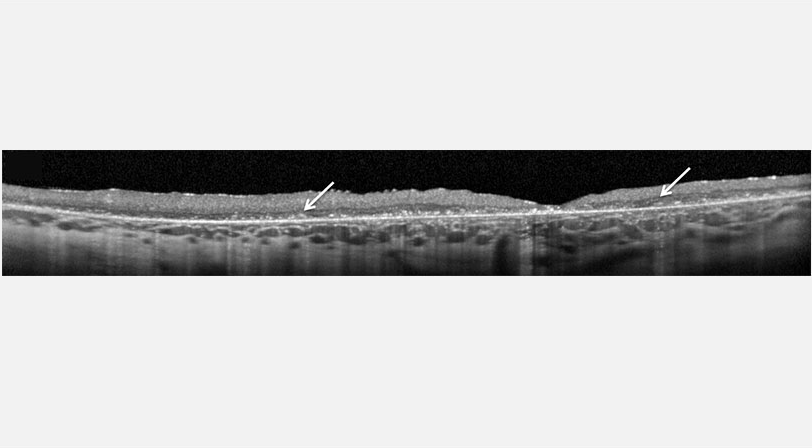
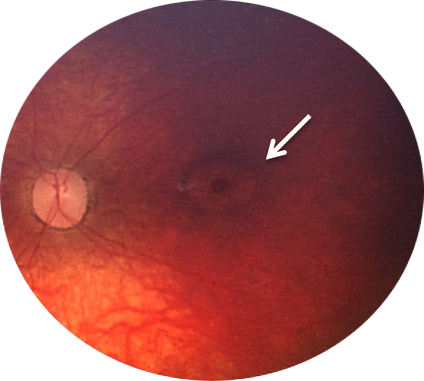
References: 1. Chang M et al. CLN2. In: Mole S, Williams R, and Goebel H, eds. The neuronal ceroid lipofuscinoses (Batten Disease). 2nd ed. Oxford, United Kingdom: Oxford University Press; 2011:80-109. 2. Mole SE et al. Correlations between genotype, ultrastructural morphology and clinical phenotype in the neuronal ceroid lipofuscinoses. Neurogenetics. 2005;6:107-126. 3. Albert DV et al. Unique Characteristics of the photoparoxysmal response in patients with neuronal ceroid lipofuscinosis type 2: can EEG be a biomarker? J Child Neurol. 2016;31:1475-1482. 4. Fietz M et al. Diagnosis of neuronal ceroid lipofuscinosis type 2 (CLN2 disease): Expert recommendations for early detection and laboratory diagnosis. Mol Genet Metab. 2016; 119:160-167 5. Mole SE and Williams RE. Neuronal ceroid-lipofuscinoses. 2001 Oct 10 [Updated 2013 Aug 1]. In: Pagon RA, Adam MP, Ardinger HH, et al., editors. GeneReviews® [internet]. Seattle, WA: University of Washington; 1993-2016. 6. Orlin A et al. Spectrum of ocular manifestations in CLN2-associated Batten (Jansky-Bielschowsky) Disease correlate with advancing age and deteriorating neurological function. PLoS One. 2013;8:e73128. 7. Williams RE et al. Management Strategies for CLN2 Disease. Pediatr Neurol 2017;69:102–112.
 UK (English)
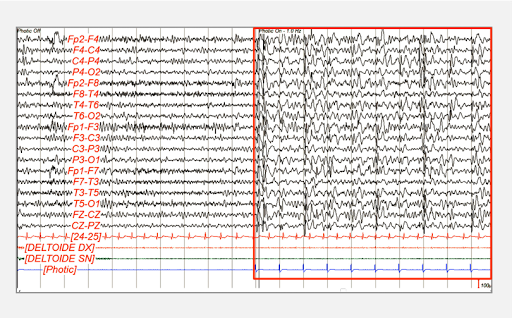
UK (English)
 Español
Español Türkçe
Türkçe Deutsch
Deutsch Italiano
Italiano Русский
Русский Français
Français